Provident has been engaged in ongoing DRG audits since ICD-10 was implemented in October 2015. We have identified potential DRG audit target areas related to our audit work, changes to the ICD-10 codeset, and Coding Clinic updates. We will be posting cases regularly in our newsletter. Please see this edition’s case study below:
Case Summary
A 78-year-old female with history of hypertension comes in complaining of hematochezia since the previous night. Per ER, she was tachycardic (HR 105), hypotensive (88/32), and tachypneic (RR=22). ER impression: Major GI bleed with severe acute anemia associated with acute blood loss. Blood work showed hemoglobin of 5.7 g/dL, creatinine 3.6 which is significantly elevated with compared to her previous baseline of 1.9. GFR 12. C02 19. Anion Gap 13.
Per H&P was noted to have profound cutaneous pallor and a lower GI bleed due to active sigmoid column bleeding, transfused 3 units of PRBCs, started on dopamine drip, and was transferred to the ICU. Colonoscopy showed active bleeding from a sigmoid polyp, biopsy came back positive for adenocarcinoma.
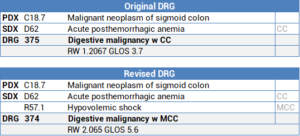
DRG Options
Note: Full listing of secondary diagnoses and procdure code assignment not shown
Audit Considerations & Strategies
- The coder correctly assigned the principal diagnosis as malignant neoplasm of sigmoid colon since the bleeding was attributed to the malignancy and acute blood loss anemia as a secondary diagnosis
- The clinical findings of severe hypotension, tachycardia, and tachypnea in setting of a major GI bleed with acute blood loss anemia, significantly elevated creatinine from baseline, low GFR, elevated bicarbonate level and anion gap support the potential diagnosis of hypovolemic shock
- Query example below:This is a 78-year-old female who comes in complaining of hematochezia since the previous night. Per ER, she was tachycardic (HR 101), hypotensive (95/32), and tachypneic (RR=20). ER impression: Major GI bleed with severe acute anemia associated with acute blood loss. Blood work showed hemoglobin of 5.7 g/dL, creatinine 3.6 which is significantly elevated when compared to her previous baseline of 1.9. GFR 12. C02
- Anion Gap 13. Per H&P was noted to have profound cutaneous pallor and a lower GI bleed due to active sigmoid column bleeding, transfused 3 units of PRBCs, started dopamine drip and was transferred to the ICU.
To ensure coding accurately reflects the severity and complexity of this case, please select from the options below:
- Patient had a lower GI bleed with acute blood loss anemia and hypovolemic shock present on admission
- Patient had a lower GI bleed with acute blood loss anemia only
- Other (please specify)
- Unable to determine
- Whenever reviewing cases with severe GI bleeds, look for clinical indicators supporting hypovolemic shock (See clinical indicators below, list is not exhaustive)
- Clinical Findings:
- Evidence of hemorrhagic and non-hemorrhagic fluid losses
- Hypotension (e.g., systolic blood pressure <90 mmHg)
- Tachycardia
- Oliguria
- Abnormal mental status
- Tachypnea
- Cool, clammy, cyanotic skin
- Labs
- Severe anemia
- Metabolic acidosis
- Hyperlactatemia
- Treatment:
- IV fluid boluses (e.g. 500 to 1000 mL)
- Vasopressors
- Adrenergic agonists (e.g. Levophed)
- Inotropic agents (e.g. Dobutamine)
References
- Healthline.com, https://www.healthline.com/health/hypovolemic-shock
- Emedicine.medscape.com, https://emedicine.medscape.com/article/760145-overview
